island health residency Program Curriculum
our curriculum & our program’s learning outcomes
- Providing evidence-based direct patient care as a member of interprofessional teams (Standard 3.1)
- Managing and improve the medication-use system (Standard 3.2)
- Exercising leadership (Standard 3.3)
- Exhibiting the ability to manage one’s own practice of pharmacy (Standard 3.4)
- Providing medication and practice-related education (Standard 3.5)
- Demonstrating project management skills (Standard 3.6)
duration of program and length of Curriculum components
| Residency Rotations & Activities | Duration | Notes |
|---|---|---|
| General Orientation | 1 Week | Meet the Department, Orientation to Residency & Organization |
| Summer Didactics (UBC) | 1 Week | Evidence Based Medicine Topics |
| Clinical Orientation on Ward | 2 Weeks | Introduction to Ward Based Clinical Pharmacy Practice |
| Direct Patient Care Rotations | 32 Weeks | Available Across a Wide Range of Clinical Specialties. Includes Precepting Rotation |
| Non-Direct Patient Care Rotations | 3 Weeks | Academic Detailing, Med Safety, Med Use Management, Pharmacy Informatics, Toxicology |
| Leadership-Management | One Full Day Workshop Plus Project | Project is Pharmacy Conference Organization. Workshop is in person. |
| Medication Use Systems | 3 Weeks | Drug Distribution & Sterile Products |
| Residency Project | 8 Weeks | Dedicated Time for Project Work |
| Vacation | 4 Weeks | |
| Total Length of Program | 54 Weeks |
Requirements to successfully complete program
Below are the required combination of rotations, both mandatory and elective to successfully complete program. Also listed are other residency program components needed to successfully complete program.
mandatory direct patient care rotations
elective direct patient care rotations
In the pre-residency survey residents rank their desired elective rotations.
These rotations are then assigned based on preceptor availability and scheduling considerations.
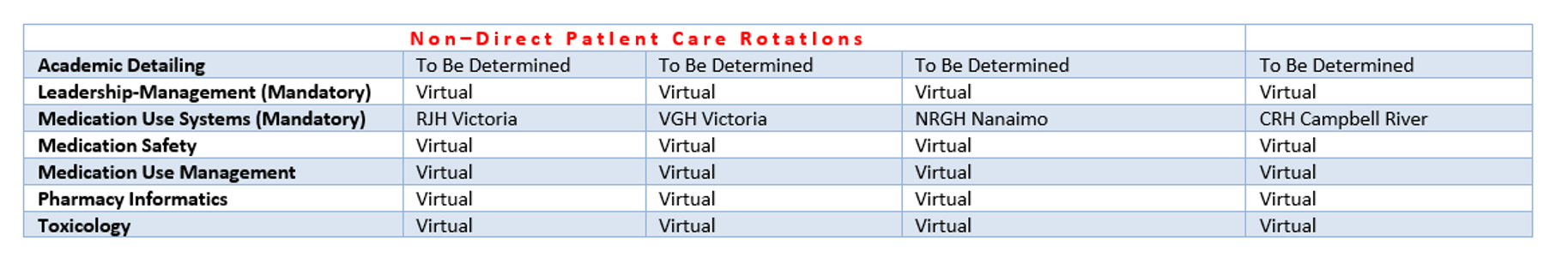
Non-Direct Patient Care Rotations
Over the residency year there are three weeks available for non-direct patient care rotations, exclusive of the leadership-management rotation. There are four one week rotations and one two week rotation to choose from. Incoming residents will rank their preferences for these rotations which will then be assigned my the residency coordinator. Residents will complete either three one week rotations or one one-week rotation and one two week rotation.
Non-Direct Patient Care Rotations. Residents Rank Preferences and Are Assigned 1 or 2 Week Rotations for a Total of 3 Weeks
Physical Location of Residents & Rotations
Resident PODs
Residents will be assigned to one of four PODS based at either the Royal Jubilee Hospital (Victoria), the Victoria General Hospital (Victoria) and the Nanaimo Regional General Hospital (Nanaimo) or North Island Hospitals (Campbell River/Comox). Incoming residents will rank their preference for POD assignments. The residency coordinator will then determine POD assignments based on survey results.